Before exam starts:
- Wash your hands
- Inroduce yourself
- Ask patient name and date of birth
- Ask the patient if it is ok that you take a look at their chest (if they are not so already, expose the chest as much as possible), and say that you will be having a listen and feel of the chest.
- NB For female patients, it would not be inappropriate to offer a chaperone at this point
- Make sure the patient is lying with their back at 45° on the bed.
General Examination
- Start with inspection of the hands
- Clubbing- cyanotic heart disease/chronic pulmonary hypertension
- Splinter haemorrhage- rare sign of infective endocarditis
- Tar staining
- Tendon xanthomata (lipid deposits)- hypercholesterolaemia
- Leukonychia- anaemia
- Capillary refill of the nail bed- anaemia/hypotension
- Cyanosis- heart failure
- Osler’s nodes (painful swellings on the fingers) and Janeway lesions (small pimples on the pulps of the hands)- infective endocarditis
- Deformity- rheumatoid disease (may be multi-system)
- Pulses (Bilateral)
- Rate, rhythm, volume, character
- To assess a collapsing pulse, take the radial pulse normally then raise the arm to see if it disappears (sign of aortic insufficiency- most commonly regurgitation).
- If there is a discrepency in the timing of pulses: sign of coarctation of the aorta (may be an emergency)
- Radial – radial : coarctation proximal to the left subclavian artery
- Radial – femoral : distal to the left subclavian
- If there is a discrepency in volume?
- Blood pressure
- May require assessment of orthostatic hypotension (lying/standing BP)
- Discrepencies between arms – may be a sign of coarctation or aortic dissection
- JVP
- Turn head up and to the side. Normally no JVP seen.
- Use the hepatojugular reflex (apply upward pressure on the liver) to exaggerate the JVP if necessary
- JVP is raised in right-sided heart failure, typically due to pulmonary hypertension or tricuspid stenosis (occasionally regurgitation too).
- Turn head up and to the side. Normally no JVP seen.
- Carotid Artery
- Feel for and assess pulse
- Auscultate for bruits (sign of arterial disease)
- Face
- Look at the eyes for xanthalasma and corneal arcus (cholesterolaemia), pale conjunctiva (anaemia).
- Look at the tongue for beefiness (anaemia), pallor/cyanosis (anaemia/hypoxia due to heart failure).
- Pallor/cyanotic lips or flush (malar flush may be seen in mitral stenosis)
- Inspection of the chest
- Look for scars, deformity, presence of hair, visible pulsations etc.
- Palpate the chest
- For apex beat, begin by using the flat of your hand around the area (5th intercostal, mid-clavicular line) before using your fingers to pinpoint the location. Strength, rate and rhythm, again.
- Place the flat of your hand over the left parasternal edge, pointing towards the neck, to feel for a left parasternal heave (movement of the hand with every beat- indicative of right ventricular hypertrophy.
- Using the flat of your hand and the pulps of your fingers separately, feel at the apex, upper part of the praecordium and in the sternal notch for thrills (palpable murmurs- most commonly aortic stenosis).
- Auscultation of the praecordium
- Auscultate with the bell and the diaphragm of the stethoscope in all four valve areas (All Prostitutes Take Money).
- Ask the patient to turn to their left side and exhale and listen with the bell at the 4th IC space just medial to the axillary line for a mid-diastolic murmer of mitral stenosis.
- Auscultate in the axilla with the diaphragm for radiation of a systolic murmur (pan-systolic murmur of mitral regurgitation).
- Ask the patient to sit forward and exhale to listen, with the diaphragm at the left parasternal edge, for a diastolic murmur of aortic regurgitation.
- Auscultate the carotid arteries too for aortic stenosis or carotid artery disease.
- Auscultate the lung bases briefly for fluid in the lungs.
You would also want to
- Palpate the abdomen for the aorta and any masses of abdominal aortic aneurysm
- A pulsatile mass may be a structure overlying the aorta and may not be significant
- An expansile mass (i.e. expands/contracts) is usually a significant finding
- Don’t push too hard if you expect an AAA!
- check for oedema in the sacrum and ankles
- press down on the skin for several seconds and check if pitting (i.e. leaving an indent) is present- sign of fluid overload/heart failure or increased vascular permeability or nephrotic syndromes/hyperproteinaemia
Neurovascular (peripheral) examination
General Principles
Note that a full neurovascular exam is not always required for evaluating vascular problems. In the trauma setting, however, a full examination is important. Whilst the upper limbs and lower limbs will be examined differently (different nerves, joints etc), there are several general things that can apply to both.
- Always perform the examination in context of the history e.g. if someone comes in after falling off a wall with a ?fractured humerus- it is not appropriate to assess full range of movement or power of elbow movements (it may, however, be appropriate to assess hand movements to check for nerve damage)
- Inspect
- Look for colour difference between affected side/non-affected side (or a general abnormal colour) e.g. pale/white, erythematous/red, cyanotic/blue etc; mottled or continuous
- Look at the appearance of the limb- are there any obvious swellings, deformities, wounds or ulcers, lack of hair
- If there are wounds/ulcers- describe them e.g.
- Location (above or below the ankle); Shallow/deep/punched out; regular/irregular; clearly demarcated/uncertain border; erthematous or not; painful/tender or not; any exudate/slough
- If there are wounds/ulcers- describe them e.g.
- Any hair loss? Describe the appearance of the skin (e.g. shiny, atrophic, pigmented)
- Look specifically at the digits and between them, looking for any nail changes.
- Palpate
- Feel the temperature of the limbs with the back of your hand. Compare sides
- Feel along the major bones and compartments
- Palpate the peripheral pulses (usually distally first)
- Upper limb
- radial, ulnar and brachial
- Lower limb
- Dorsalis Pedis
- Place your fingers half way down the dorsum of the foot on the bony area in the line between the first and second toes. The bones you can feel are the dorsal aspect of the navicular and the intermediate cuneiform bones. The pulse is palpated where the artery passes over this area
- Posterior Tibial
- Locate the medial malleolus. 2-3cm below and behind it you should find the posterior tibial pulse. when taking the pulse on your own foot it is easier to use the thumb. In clinical practice the pulse is palpated using the pulps of the index and middle fingers. The artery is slightly deeper placed than the dorsalis pedis and therefore more concentration is often required to feel its pulsations.
- Popliteal
- Ask the subject to bend the knee so that it is flexed to about 90 degrees. Sit on the right hand edge of the bed close to the subject right foot. As before gently clasp the sides of the knee (of either limb) and press the pulps of your fingers into the popliteal fossa.
- Femoral
- Locate the superior border of the pubis in the mid line of the body; this is the uppermost part of the pubic symphysis. Feel the anterior limit of the iliac crest. The femoral pulse can be found midway between these two bony points (the mid-inguinal point)
- Dorsalis Pedis
- Upper limb
- Test also capillary refill
- Test sensation (with cotton wool and/or pin-prick) for peripheral nerve function i.e. NOT dermatomes (although if you suspect spinal damage then dermatomes are useful)
- In the upper limb- a good way to test nerve function is to test the three main nerves which supply sensation to the hand:
- The ulnar nerve supplies innervation to the medial aspect of the hand (little finger/hypothenar eminence)
- The median nerve supplies innervation to the palmar aspect of the index finger and the middle palm
- The radial nerve supplies innervation to the lateral aspect of the hand (particular over the dorsum of the hand)
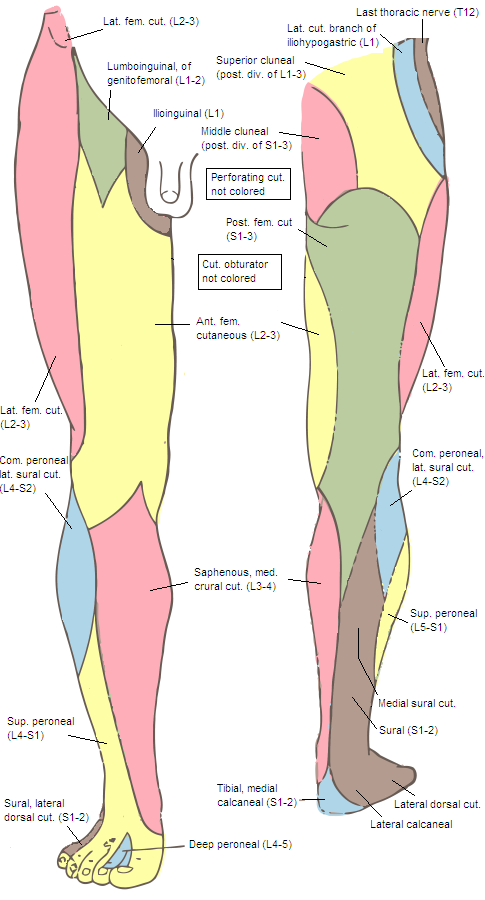
- In the lower limb, a similar approach can be taken:
- Test the femoral nerve via the medial aspect of the thigh (ant cut fem) and calf (saphenous nerve)
- Test the sciatic nerve via the lateral calf and dorsum of the foot (tibial -> sural nerve); and the webspace between the 1st and 2nd toes (common peroneal -> deep peroneal nerve)
- The obturator nerve may be tested via the distal medial thigh
- Ask about pins and needles
- Check for any pitting oedema by pressing with your thumb for several seconds. A ‘thumbprint’ will remain on the area if pitting oedema is present.
- Movements
- Where appropriate, test active and passive movements and power of the appropriate limbs. If there is any pain or weakness, document this.
- Disproportionate pain on passive extension (/stretch) will tend to suggest compartment syndrome
- DO NOT TEST PASSIVE MOVEMENT ON AN OBVIOUSLY INJURED LIMB – this may cause further damage
- NB You could test movement distal to an injury to evaluate nerve damange
- In the lower limb-
- Peroneal nerve- foot dorsiflexion
- Tibial nerve- foot plantar flexion
- In the upper limb-
- Radial nerve- Extension of the hand joints and wrist
- Ulnar nerve- Abduction of the fingers
- Median nerve- thumb opposition (also wrist flexion)
- Where appropriate, test active and passive movements and power of the appropriate limbs. If there is any pain or weakness, document this.
Ankle Brachial Pressure index:
- Procedure
- Using the sphygmomanometer and stethoscope, measure the blood pressure on the arm (brachial pressure). Alternatively (more common at present), use a doppler USS and the sphygmomanometer to more accurately measure systolic BP
- Place the cuff above the ankle and repeat but using either the posterior tibial or dorsalis pedis pulses.
- Calculating
- ABPI (R) = Highest SBP in (R) foot / Highest SBP of either arm
- Interpretation
- <0.9 suggests PAD
- >1.4 suggests heavily calcified vessels (without PAD)
- <0.5 suggests severe PAD
- NB There may be a mix of calcification and PAD